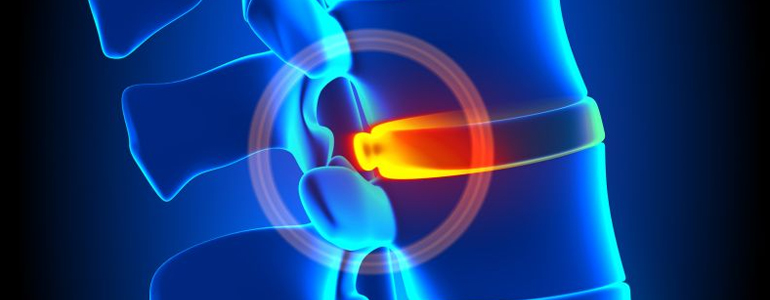
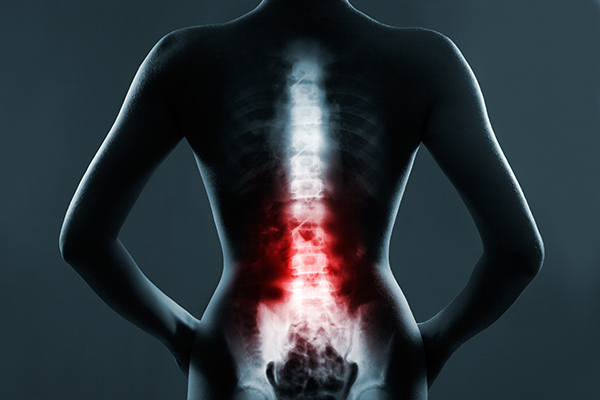
Why Minimally Invasive Spine Surgery: The purpose of minimally invasive spine (MIS) surgery is to stabilize the vertebral bones and joints, as well as relieve pressure on the spinal nerves, which is typically caused by disorders including spinal instability, bone spurs, herniated discs, scoliosis, or malignancies.
Minimally invasive surgical methods can be quicker, safer, and need less recovery time than open spine surgery. The possible benefits are as follows: Less stress to the muscles and soft tissues (as compared to open procedures): Let’s know more about Why Minimally Invasive Spine Surgery.

- Conditions Treated Using MIS Procedures
- How Minimally Invasive Spine Surgery Works
- Using a Tubular Retractor
- Common MIS Surgery Treatment Options
- Candidates for MIS Surgery
- Glossary of Select Spine-Related Surgical Terms
- Device Technology
- Spinal Fusion
- MIS Fusion Procedures
- Minimally Invasive Spine Surgery At Gwalior

- Skin incisions that are tiny produce better aesthetic outcomes (sometimes as small as several millimeters)
- Surgery results in less blood loss.
- Muscle injury is less likely since less or no muscle cutting is necessary.
- Infection risk and surgical discomfort are reduced.
- Surgery recovery is quicker, and rehabilitation is less time-consuming.
- After surgery, there is less dependency on pain drugs.

Furthermore, certain MIS treatments are conducted as outpatient operations with just local anaesthetic, reducing the risk of a negative reaction to general anaesthesia. Let’s know more about Why Minimally Invasive Spine Surgery.
There are dangers connected with every surgical operation, no matter how little, which include, but are not limited to:
Anesthetic side effects are a possibility.
During the surgery, there was unexpected blood loss.
No matter how tiny the incision area, localised infections might occur.
And, while it’s rare, there’s always the possibility that the initial MIS surgery may fail, necessitating either a second treatment or full open surgery.

Conditions Treated Using MIS Procedures
- Degenerative disc disease (DDD) is a kind of degenerative
- Disc herniation
- stenosis of the lumbar spine
- Scoliosis is a type of spinal deformity.
- Infections of the spine
- Spondylolisthesis is a kind of spinal instability.
- Compression fractures of the vertebrae
- Tumors of the spine

How Minimally Invasive Spine Surgery Works
Due to the location of the spinal nerves, vertebrae, and discs deep within the body, any strategy to obtain access to the spinal region necessitates the removal of muscle tissue. This is often accomplished by making small incisions and directing equipment and/or microscopic video cameras through them. Lasers are rarely employed in MIS operations, contrary to common assumption. Let’s know more about Why Minimally Invasive Spine Surgery.

During MIS surgery, a variety of techniques can be employed to reduce trauma. The following are some of the most frequent approaches.
Using a Tubular Retractor
Rather of cutting directly through the muscles, this approach includes gradual dilatation of the soft tissues. The surgeon can work through the incision without having to expose the region too much by utilising tubes to keep the muscles out of the way. An endoscope or microscope directed down the tube may be utilised by the surgeon to aid in executing the operation using a limited access technique. The tubular retractor can be withdrawn when the treatment is finished, enabling the dilated tissues to heal. Incisions can vary in size depending on the degree and kind of surgery required.
Percutaneous Placement of Screws and Rods
Read More:
Depending on the patient’s condition, instrumentation like as rods and screws may be used to support the spine or immobilise the spine to aid in the fusing of the spinal bones. Traditional screw placement methods need substantial muscle and other tissue removal from the spine’s surface.
Percutaneous (meaning “through the skin”) implantation, on the other hand, often entails introducing rods and screws through tiny skin incisions rather than cutting or dissecting the underlying muscle. Guidewires are inserted through the skin and into the spinal vertebrae along the intended screw pathways using x-ray pictures. The guidewires are then covered with screws that follow the wires’ course. Let’s know more about Why Minimally Invasive Spine Surgery.
These screws feature temporary extenders that extend outside of the skin and are removed after assisting in the connection and securement of the screws by guiding the passage of rods. Spinal instrumentation is being implanted more safely and correctly because to the use of spinal navigation and robotics.
Direct Lateral Access Routes

Because there is less muscular tissue blocking the route in some situations, especially those involving the lumbar spine, accessing the spine from the side of the body might result in less discomfort. The patient is usually on his or her side throughout this procedure. Then, on the side of the spine, a tubular retractor docks to provide access to the spine’s discs and bones. Let’s know more about Why Minimally Invasive Spine Surgery.
Thoracoscopic Access Route
It may be essential to reach the front sections of the thoracic spine, which are positioned in the chest and are surrounded by the heart and lungs, depending on the patient’s condition. Traditional access methods frequently include making major incisions in the chest, which may need the removal of one or more ribs. Thoracoscopic access, on the other hand, relies on a series of tiny incisions through which functioning ports and cameras can be introduced to aid operation. Let’s know more about Why Minimally Invasive Spine Surgery.
Common MIS Surgery Treatment Options
For MIS surgery, a variety of particular approaches have been used. Despite the fact that the area is still evolving, the list below illustrates some of the most frequent alternatives.
Discectomy: Spinal discs are elastic rings filled with soft material that act as cushions between the spinal bones. The soft tissue inside the elastic ring might protrude — or herniate — outside of the ring if it gets weaker. The debris from a herniated disc might compress nearby nerves, producing discomfort. If surgery to trim or remove the herniated disc is recommended, it may be possible to do so with MIS surgery employing tubular dilators and a microscope or endoscope. Let’s know more about Why Minimally Invasive Spine Surgery.
Spinal decompression:The narrowing of the vertebral canal, known as spinal stenosis, is a frequent disorder that can cause nerve compression. Pain, numbness, and muscular weakness are some of the symptoms that might result. If surgery is necessary, a MIS technique employing tubular dilators and a microscope or endoscope may be used to remove the bone and soft tissues that are causing the nerve compression. Laminectomy and foraminotomy are two of the most popular decompressive surgeries.
Transforaminal Lumbar Interbody Fusion (TLIF): Patients with persistent mechanical low back and radicular pain linked with spondylolisthesis, degenerative disc disease, and recurrent disc herniation are treated with this MIS approach. With the patient on his or her stomach, the surgery is conducted from the back (posterior). Screws and rods are put between two or more spinal levels using two tiny incisions. The intervertebral disc is removed, and a bone cage is inserted in its place, with the purpose of stabilising the afflicted levels. Let’s know more about Why Minimally Invasive Spine Surgery.
Candidates for MIS Surgery
A doctor will be able to determine which, if any, MIS operations are appropriate for treating a spinal issue. MIS surgery may not be as safe or successful as regular open surgery in some cases. If this is the case, the doctor will be able to explain the risks and advantages to you. Furthermore, certain illnesses are not completely curable with MIS surgery. Let’s know more about Why Minimally Invasive Spine Surgery.

Glossary of Select Spine-Related Surgical Terms
- Bone spur: Rough margins of bone or bony growth (a.k.a. osteophyte).
- Decompression: A surgical treatment used to reduce pressure and discomfort caused by bone and/or disc material impingement on the spinal cord or nerves.
- Disc degeneration: A disc’s degeneration or wear and tear. Over time, a disc in the spine may degrade or wear out. Pain may or may not be caused by a damaged disc.
- Discectomy: Part or all of an intervertebral disc is surgically removed to alleviate pressure on a nerve root or the spinal cord.
- Excision: As with removing a disc, removal is accomplished by cutting away material.
- Facet: A facet joint is a vertebra’s posterior structure that articulates (joins) with a facet of a neighbouring vertebra to facilitate mobility in the spinal column. Each vertebra has a superior (upper) and inferior (lower) facet on the right and left sides.
- Foramen: The spinal nerve roots pass through this hole or channel in the vertebrae of the spine on a regular basis.
- Foraminotomy: Surgically enlarging or widening the bone aperture passed by a nerve root as it exits the spinal canal to allow that nerve have more room.
- Herniated disc: A disorder in which the gelatinous core material of a disc bulges out of place and puts excruciating pressure on surrounding nerve roots, commonly known as a slipped or ruptured disc.
- Intervertebral foramen: Nerves exit the spine and go to different regions of the body through this hole between vertebrae. Also referred to as the neural foramen.
- Kyphosis: A condition in which the upper back bends forward, resulting in the appearance of a back hump. Kyphosis can be caused by years of bad posture, osteoporosis-related spine fractures, trauma, or developmental issues.
- Lamina: The ceiling of the spinal canal is formed by the flattened or arched section of the vertebral arch.
- Laminectomy: Surgically removing the back half of a vertebra to provide access to the spinal cord or nerve roots, remove malignancies, repair spine injuries, or alleviate pressure on a nerve root.
- Laminotomy: An opening in a lamina that allows pressure on the nerve roots to be relieved. Unlike a laminectomy, which removes the complete lamina, a laminotomy usually only removes half of the lamina (the side where a patient is having symptoms).
- Lordosis: The inward curvature of the lumbar spine is referred to as lordotic curves. This might be a spinal malformation, also known as swayback, which happens when the lower back bends inward more than normal in certain people. Osteoporosis or spondylolisthesis can produce pathologic or excessive lordosis. Obesity, congenital abnormalities, or kyphosis overcompensation may all play a role in this illness.
- Medial facetectomy: A treatment in which a portion of the facet is excised in order to enhance spinal canal space.
- Nerve roots: The nerve root is the first segment of a spinal nerve; it is a central nervous system extension that originates in the spinal canal and terminates in the extremities (fingers, toes). Its function is to transmit sensory information from the extremities to the brain, as well as motor orders from the brain to the extremity.
- Pedicle: The bony portion of either side of a vertebra’s neural arch that joins the lamina (back section) to the vertebral body (front part).
- Percutaneous: Through the skin, something is effected, happens, or is done.
- Pseudarthrosis: Movement of a bone at the site of a fracture or fusion due to insufficient fracture healing or failure of the fusion to develop appropriately. A developmental failure might potentially cause this.
- Scoliosis: The spine has a lateral (sideways) curvature.
- Spinal stenosis:Pressure on the spinal cord, spinal sac, or nerve roots originating from the spinal cord due to abnormal constriction of the vertebral column.
- Spinous process: Muscles and ligaments are linked to a thin protrusion of bone from the rear of a vertebra.
- Spondylitis: Vertebral inflammation.
- Spondylolisthesis: The movement of one vertebra forward on another.
- Spondylosis: The intervertebral discs and facet joints are most typically affected by degenerative changes in the spine.
Device Technology
- Endoscope: A tiny, fiberoptic tube with a light and lens that is used to view the inside of a patient’s body; it allows for minimally invasive diagnostic and surgical operations.
- Fluoroscope: Intraoperatively, an imaging equipment that employs x-rays to observe interior body features on a screen.
- Laparoscope: An tool that allows you to see certain structures in your body. The laparoscope is implanted through a tiny surgical incision. A series of tubes can be routed via the same or other tiny incisions, allowing probes and other tools to be used.
- Minimally invasive tubular retractor (MITR): Muscle-splitting surgery was initially used in combination with microendoscopic discectomy in 1995. The tubular retractor is a device that is used to build a tunnel down to the spinal column and can be as tiny as 1.4 cm in diameter (approximately 1/2 inch). The tubular retractor is inserted via a tunnel in the back muscles, rather than tearing the muscles away from the spine, as is done in open operations. This method protects the muscles around the spine and reduces blood loss during surgery.
- Portals: During endoscopic operations, devices that offer a route through which the surgeon can work. Dilators are utilised to access the region of the spine where the surgeon is operating after the incision is created. At the time of operation, fluoroscopy is utilised to find the correct level. Instruments are utilised to continue the dissection via the portal during the surgery.
- When the portal is removed, all of the tissue returns to its original position. The portal or tubular retractor is put into the incision to keep the tissue apart and is retained in place during the surgery to avoid injuring the tissue by moving devices in and out of the route. There are portals that are open and portals that are closed. Portals utilised in the thoracic spine are typically 11 to 12 mm in diameter, but portals used in the abdominal cavity are often bigger. All devices and implants must be engineered to fit through these narrow pathways and execute surgical tasks once they get at their destination.
Spinal Fusion
A spinal fusion is a procedure that joins two or more vertebrae together permanently. This operation can help to strengthen and stabilise the spine, which can help to relieve severe and persistent back pain.
The implantation of a bone graft between the vertebrae is used in almost every surgical treatment option for fusing the spine. Bone grafts can come from the hip or another bone in the same patient (autograft), or they can come from a bone bank (allograft). Bone graft extenders and bone morphogenetic proteins (hormones that allow bone to develop within the body) can also help to lessen or eliminate the need for bone transplants.
Supplementary hardware (instrumentation) such as plates, screws, and cages may or may not be used during fusion. The fusion of the bone transplant with the spine’s bones will create a permanent bond between them. The hardware is no longer required after that, but most patients decide to keep it in place rather than undergo another operation to remove it. MIS procedures can occasionally be used to accomplish fusion with fewer incisions. Advanced fluoroscopy, endoscopy, and navigation have increased the precision of incisions and hardware implantation, reducing tissue stress and allowing for a MIS approach.

MIS Fusion Procedures
- Invasiveness is kept to a bare minimum. Fusion of the Lateral Interbody
- Invasiveness is kept to a bare minimum. Interbody Fusion of the Posterior Lumbar Spine (PLIF)
- Invasiveness is kept to a bare minimum. Lumbar Transforaminal Interbody Fusion (TLIF)
- Posterior Thoracic Fusion with Minimal Invasiveness
The KLM GROUP does not recommend any of the therapies, techniques, products, or practitioners mentioned in these patient info sheets. This material is offered solely for educational purposes and does not constitute medical advice. Anyone wanting particular neurosurgical advice or help should visit their neurosurgeon, or use the AANS’ Find a Board-certified Neurosurgeon” online service to find one in your region.
Minimally Invasive Spine Surgery At Gwalior
Dr Vipin the managing director of KLM Group. He is a well-known gold-medalist Orthopedic Surgeon In gwalior, strongly reputed for his trusted and focused attitude our rich knowledge and experience, be assured of quality healthcare and world-class medical services in Orthopaedic, Spine care In gwalior, Ophthalmology, X-ray & Diagnostics services along with physiotherapy services.
Address: 12, Saraswati Nagar, University Road, Near Silver Estate, Thatipur, Gwalior 474006 Mob: 7804826825 Ph: 0751-4000721 Website: www.klmgroup.org Email: info@klmgroup.org / klmspineclinic.in@gmail.com

